Diastasis Recti: How to Prevent and Treat Abdominal Separation
- Janine Laughlin, physical therapist, clinic owner
- Feb 24, 2016
- 5 min read
Updated: Apr 16, 2024
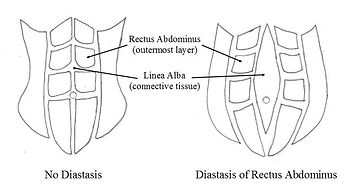
Diastasis recti abdominus (DRA) is a separation of the rectus abdominus along the linea alba, typically measured in finger widths and more recently, inter recti distance (IRD). It is more common in women as a result of abdominal wall distention in pregnancy, although men can have it also. According to Diane Lee, Canadian physiotherapist, 100% of women have some level of DRA in the third trimester (Diane Lee, 2013). It is estimated that 66% of women have some level of pelvic floor dysfunction associated with diastasis recti (Spitznagle et al, 2007) that can contribute to urinary, bowel and/or sexual dysfunction. In addition, for many postpartum women whose abdominal wall remains unclosed at 8 weeks, the gap remains unchanged at one year, if left treated (Coldron et al, 2008, & Liam et al, 2011). This means the problem will not go away on its own as many women are told. Furthermore, pelvic girdle pain affects 45% of women during pregnancy and 20-25% in the early postpartum period (Wu et al, 2004). With this knowledge, every woman should receive a postpartum evaluation by a pelvic health physical therapist.
We believe prevention of diastasis recti begins DURING pregnancy and we recommend assessing the integrity of the abdominal wall before beginning an exercise program in the postpartum period. Often the rectus abdominus separates like a zipper along the linea alba (vertical ligament dividing the rectus muscles that becomes discolored in pregnancy) as the pregnancy advances. Although many will tell you it will close on its own, the gap can remain and worsen over time as a result of the increased stress placed on it from exercise and/or improper lifting.
The problem with diastasis recti is not the gap itself but the improper recruitment and timing of the deep core muscles, increasing the risk for other conditions such as low back pain, pelvic organ prolapse and urinary incontinence. If the deep core muscles are not restored to function, increases in intra-abdominal pressure, such as during coughing, lifting or abdominal exercise, can result in symptoms of overload. In addition, co-activation of all four deep core muscles is required to transfer loads effectively through the lumbopelvic region during daily tasks (Hodges et al, 2007). Many women treated in our clinic come in with a complaint of low back pain and urinary leaking and have had unresolved DRA even though their child was born several years ago. Once the diastasis is addressed, these symptoms go away. We also have patients who have unresolved back pain and urinary leaking due to the abdominal separation. Modification of exercise and activity is necessary, along with retraining the deep core system.
PREVENTING DIASTASIS RECTI
Prevention of DRA begins during pregnancy, which is one reason we recommend an evaluation by a women's health therapist BEFORE and DURING pregnancy, especially if dysfunctions are already present. Understanding pressure management and learning how to engage the deep core muscles simultaneously is paramount. One way this can be accomplished is by EXHALING every time you lift something or yourself. For example, getting out of a chair, picking up the infant carrier, lifting groceries or weight training. The deep core muscles are activated on the exhale. It is also helpful to roll to your side when getting in and out of bed, using your arms and EXHALING to sit up (example below). Learn how to engage the deep core or modify the exercise/activity, especially if you develop symptoms of overload such as urinary leaking or prolapse. Supporting the abdominal wall with kinesiotape can be helpful if you are impatient getting into that new high-intensity exercise class.


CHECKING FOR DIASTASIS RECTI
Lie on your back and place your fingers horizontally in your abdomen at the level of your belly button. As you lift your head, the muscles should come together and push your fingers out of the way. If you have a separation, your fingers will fall into a divot and you will feel the muscles separate. You might also see a tenting or coning at the midline, which is a concern if the pressure is firm and not soft. Check for a separation at, above and below the navel. Objective standards are still being developed as to what constitutes a diastasis recti and further research is being done.

KINESIOTAPING FOR DIASTASIS RECTI
Kinesiotape can be used to guide the muscles toward the midline without disrupting normal muscle function and a physical or occupational therapist or trainer can teach you how to apply it. Kinesiotape can be purchased at a local drug store or through your physical therapist or provider. Rock Tape is the brand we use at Healthy Core for its superior elastic and adhesive properties. If your skin is thin and frail, we recommend Rock Tape Rx. Tape can stay on for up to five days as long as your skin is not irritated. Take caution not to expose it to heat (let it air dry after showering or bathing) or it will adhere to your skin and be very difficult to remove later. Contact us to learn the best way to tape your abdomen.
TREATMENT FOR DIASTASIS RECTI
There are many things that factor into abdominal separation. Hip and spinal mobility, ribcage alignment, hip strength, breathing mechanics...are all important considerations to address if there is dysfunction. Manual therapy such as visceral mobilization can improve abdominal wall integrity and core muscle activation. The focus of exercise in the postpartum period should be on retraining the timing and sequencing of the deep core muscles that work as a team during exhalation and are often disrupted from the changes in pregnancy. We no longer give absolutes or Do's and Don'ts as loading the connective tissue can aid in its recovery and function, if done properly and if the contents are not firmly pressing outward. Plank exercises for example, can be modified instead of avoided altogether. Glute strengthening is helpful along with addressing ribcage mobility to maximize abdominal muscle function. A qualified pelvic health therapist can evaluate you with a customized approach and guide you in the most appropriate exercise program for you.
In some cases, surgery may be necessary to close the gap, however rehab including core training and addressing pelvic alignment will still be necessary to regain proper muscle function. Surgery increases the risk of adhesions, further disrupts core motor control and in some cases may be considered "cosmetic" and not covered by insurance. According to many experts including physiotherapist Diane Lee (Lee 2007), surgery should only be considered after one year of conservative treatment and the following:
IRD (inter recti distance) > mean values (15 mm) with noticeable stretch damage to abdomnal wall (Beer et al, 2009)
Abdominal contents can be palpated through midline fascia
Lack of progress with an individualized core exercise program
Unable to gain pain-free function
Unable to regain urinary continence
Diastasis recti will not likely go away on its own and increases the risk for other problems. The good news is that help is available! Contact Healthy Core or a qualified women's health pelvic therapist in your area for an evaluation so you can get back to regular activity and function optimally as the mom you were meant to be!
References:
Coldron Y, Stokes MJ, Newham DJ, Cook K (2007). Postpartum characteristics of rectus abdominis on ultrasound imaging. Manual Therapy, epub.
Hodges P, Cholewicki J (2007). Functional control of the spine. Movement, Stability & Lumbopelvic Pain. Chapter 33
Lee, DG 2004. The Pelvic Girdle, 3rd edition.
Spitznagle TM, Leong FC, van Dillen LR (2007). Prevalence of diastasis recti abdominis in a urogynecological patient population. Int Urogynecology J 18:3.
Wu WH, Meijer OG, Uegaki K, Mens JM, Van Dieen JH, Wuisman PI et al (2004). Pregnancy-related pelvic girdle pain (PPP), I Terminology, clinical presentation and prevalence, Eur Spine J 13 (7); 575-589.
written by Janine Laughlin - February 2016, revised April 2024

























